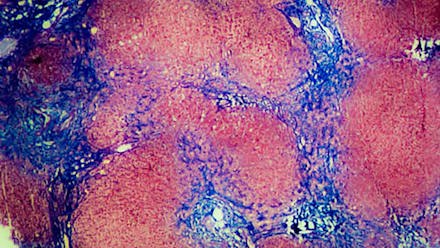
Cirrhosis
Cirrhosis occurs when healthy liver tissue is replaced by hardened scar tissue, which prevents the liver from performing many of its vital functions.
The scarring and damage to the liver builds up over time. Cirrhosis is a long-term (chronic) disease.
The leading cause of cirrhosis in the United States is alcoholism, followed by chronic viral hepatitis. It can also be caused by non-alcoholic fatty liver disease, autoimmune hepatitis and bile duct disease, and genetic diseases such as Wilson disease.
In its early stages, cirrhosis may not show any symptoms. As cirrhosis progresses, it may cause symptoms such as fatigue, fluid build-up in the abdomen (ascites), confusion, vomiting blood, gallstones, itching, yellow skin and eyes (jaundice), easy bruising, and weight loss.
How is Cirrhosis Treated?
Cirrhosis care at UC San Diego health involves a team approach. Our doctors are some of the leading liver specialists in the country and are actively involved in clinical research to provide the latest and best treatments.
Our doctors work closely with nurse practitioners who specialize in the care of liver disease, and the team collaborates to coordinate an individualized plan of care for patients with cirrhosis. We also have a robust liver transplant program.
Our liver specialists diagnose cirrhosis using a combination of methods, including reviewing a patient’s medical history, a physical exam, blood test results, non-invasive imaging methods, and possibly a liver biopsy.
The goal of treatment is to prevent further damage to the liver by changing lifestyle and diet, treating the underlying cause of liver disease, and reducing its side effects. If cirrhosis cannot be treated, a liver transplant may be recommended.
What are Complications of Cirrhosis?
We also work with you to manage the many complications of cirrhosis, including:
Portal hypertension — Cirrhosis can cause an increase in pressure to the blood vessels flowing into the liver. This can cause bleeding in the stomach, rectum and esophagus. Treatment options may include medication, endoscopic treatment to tie off bleeding blood vessels, and the placement of a transjugular intrahepatic portosystemic shunt (TIPS) to reroute blood flow and reduce pressure.
Ascites — Fluid accumulation in the abdomen occurs with portal hypertension and can be addressed with medications called diuretics or by inserting a long thin needle through the wall of the abdomen and withdrawing the fluid.
Encephalopathy — Poor liver function can affect your ability to think as toxins build up in the brain, causing confusion and forgetfulness.
Liver cancer — Cirrhosis is a form of internal scarring in the liver, and is the leading cause of liver cancer. Your doctor may recommend imaging and blood testing every six months to screen for liver cancer.Learn About our Comprehensive Liver Cancer Care
Classes & Support Groups
Education classes and support groups for people who have hepatitis C and liver cancer are available.
Learn more about the liver transplant process