The COVID-19 pandemic has killed nearly 7 million people worldwide (1.1 million in the United States) and severely harmed many millions more, though vaccines and antiviral treatments measurably reduced the potential loss of life and health.
A Commonwealth Fund report , for example, estimated COVID-19 vaccines alone prevented more than 18 million additional hospitalizations and 3.2 million additional deaths in the U.S.
The pandemic has never been simple or easy. For example, the emergence of viral variants, in particular recent versions of the Omicron, fueled new surges of infection and disease throughout 2022 and into 2023.
“There were real concerns about new waves of cases driven by BA.5, which had replaced BA.2.12.1 as the dominant strain in the United States,” said Aaron Carlin, MD, PhD, associate professor of pathology at University of California San Diego School of Medicine. “It looks like past infection by an earlier subvariant would not elicit cross-protection against the new BA.4 and BA.5 subvariants.”
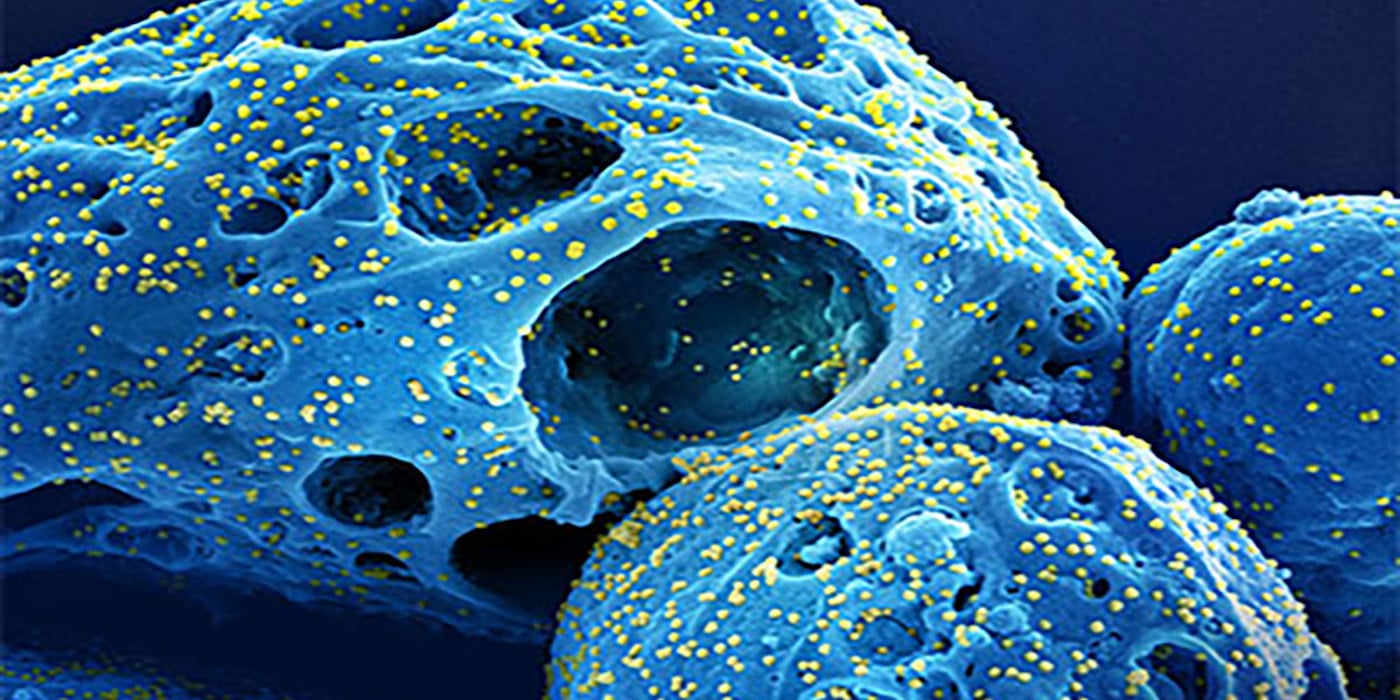
In a new study, published in the March 21, 2023 online issue of Open Forum Infectious Disease , Carlin and colleagues at UC San Diego School of Medicine describe why COVID-19 subvariants spread rapidly among people previously infected and how the popular Paxlovid therapy might have made people more susceptible to future infections.
The researchers found that mutations in the spike protein of BA.4 and BA.5 allowed it to evade neutralizing antibodies generated by vaccination or by an earlier SARS-CoV-2 infection. Moreover, they determined that early treatment with Paxlovid, an oral antiviral pill that combines drugs (nirmatrelvir and ritonavir), dampened the natural development of antibodies, leaving people with lower overall immune responses and perhaps more vulnerable to subsequent infection.
Paxlovid was among the first drugs developed and tested to treat COVID-19, and quickly became a go-to medication, often prescribed when symptoms first appeared and intended to reduce the likelihood of severe disease, hospitalization or death. Subsequent research has shown that Paxlovid treatment among non-hospitalized, unvaccinated patients at high risk of progression to severe disease reduced the risk of hospitalization or death by 88%, and the risk of long COVID.
But Paxlovid proved poor insurance against recurrence of COVID-19 or subsequent re-infection.
In June 2022, senior author Davey Smith, MD, chief of Infectious Diseases and Global Public Health at UC San Diego School of Medicine and an infectious disease specialist at UC San Diego Health, Carlin and colleagues published data suggesting the so-called “Paxlovid rebound” was likely due to insufficient drug exposure.
In October 2022, Smith and colleagues published a different study that documented the likelihood of COVID-19 symptoms recurring in untreated patients after initial symptoms had disappeared.
"Our findings suggest that while early antiviral treatment can prevent severe COVID-19, it does not obviate the need for subsequent vaccination or boosters to promote protective immune responses,” said Smith.
“The findings also highlight the importance of ongoing research and the need for continued efforts to understand the virus and develop effective treatments and vaccines. The past is prologue, not because the virus is the same, but because it is constantly changing, so we must evolve as well to meet the threat and anticipate the next pandemic.”
Co-authors include: Alex E. Clark, Aaron F. Garretson, William Bray, Magali Porrachia, Tariq M. Rana and Antoine Chaillon, all at UC San Diego; and AsherLev T. Santos, CSU San Marcos.
Funding support for this research came, in part, from the National Institutes of Health (grants AI036214, AI131385, CA177322, DA039562, DA046171, AI125103, DA049644, AI145555, MH128153, AI106039, K08 AI130381 and DP2 CA051915), San Diego Center for AIDS Research (AI100665), Department of Veterans Affairs, the John and Mary Tu Foundation and the James B. Pendleton Charitable Trust and a Career Award for Medical Scientists from the Burroughs Wellcome Fund.
Topics
COVID-19 Infectious Disease