
Bryce Bandfield was inspired to become a nurse after his brother was hospitalized for a serious illness at a young age and he witnessed first-hand how nurses positively influence a patient’s hospitalization. Photo credit: Alex Matthews, UC San Diego Health
On any given day within the walls of a hospital, many people are being impacted by once-in-a-lifetime events.
Whether it is parents welcoming a new child into the world, a person finishing their last treatment for cancer, or a family member sitting at bedside of a loved one and holding their hand through a life-threatening illness, hospital employees experience some of the most significant and emotional moments in a patient’s life.
For Bryce Bandfield, RN, these moments are what inspired him to become a nurse after his brother’s hospitalization for a serious illness at a young age.
"It was really eye-opening to see how nurses positively influence a patient’s hospitalization. With my brother they were fun, inviting and educational with him to help normalize the fact that he was in the hospital at such a young age," said Bandfield, a critical care nurse at UC San Diego Health. "This impact is lifelong, too, as the care and treatment nurses provide in the hospital forever change the trajectory of a patient’s life and their overall health."
In 2024, more than 40,000 patients were hospitalized at UC San Diego Health, the region’s only academic medical center, where more than 13,000 people work and provide care each day.
Bandfield is part of an intensive care unit (ICU) at Jacobs Medical Center at UC San Diego Health, which offers treatment for some of the most critically ill patients in San Diego. The team was recently recognized by the American Association of Critical-Care Nurses (AACN) with the Beacon Award for Excellence. The award honors health care units that distinguish themselves for providing high-quality patient care in a healthy work environment. A surgical oncology progressive care unit at Jacobs Medical Center was also recently recognized with a Beacon Award in early 2025.
The Beacon Award program comprises three distinct areas: patient outcomes, work environment and nursing workforce. For nurses, this award demonstrates a positive and supportive work environment with greater collaboration and higher morale.
Across the health system, UC San Diego Health is Magnet-accredited, offering a nationally acclaimed team of health care physicians and nurses who deeply care for our patients and their loved ones.
In this Q&A, Bandfield reflects on his time as a registered nurse and the patients he’s cared for, and he provides a first-hand view on what a typical day looks like in the ICU at UC San Diego Health.
 Bandfield is part of an intensive care unit at Jacobs Medical Center at UC San Diego Health, which offers treatment for some of the most critically ill patients in San Diego. Photo credit: Alex Matthews, UC San Diego Health
Bandfield is part of an intensive care unit at Jacobs Medical Center at UC San Diego Health, which offers treatment for some of the most critically ill patients in San Diego. Photo credit: Alex Matthews, UC San Diego Health
Why did you become a registered nurse?
When I was 20, my brother was hospitalized when he was very young and needed to stay in the hospital for quite some time. While there, I witnessed the positive effect nurses have on patients and their day-to-day moments while in the hospital. The nurses provided exceptional care for my brother and our family, too. While still dealing with a chronic illness my brother has since stabilized, but this moment in our lives solidified my career path in nursing.
I started as a certified nursing assistant (CNA), providing support to teams in the Emergency Department, perioperative care, and other units. In particular, I loved working in skilled nursing facilities. Taking care of seniors and someone else’s loved ones in a home-like setting was really where my passion in nursing began.
During my time working as a CNA, I obtained my Bachelor of Science in Nursing and worked in multiple in-patient units at local health care organizations, including UC San Diego Health. Ultimately, I knew that I wanted to work with the sickest and most vulnerable patients, and that’s what led me to the ICU.
What does a typical day in the ICU look like?
My work day starts at 7 a.m. At the beginning of each shift, our team huddles in the morning to discuss our unit’s 24 patients and individuals that need extra assistance, and I receive my assignment for the day. After huddle, I receive a report from the night shift nurse, which includes why each patient under my assignment is hospitalized, how the last shift went, what medications they are currently receiving, such as blood pressure medication, pain medication, sedation or blood thinners, what life support the patient is on, such as a ventilator, extracorporeal membrane oxygenation device (ECMO), or continuous renal replacement therapy.
We also review any labs, results and pending tests, and any other pertinent information to have a better understanding of each patient and what needs to be done during my shift.
Daily activities for my patients include simple things, like oral care and bathing. Along more complex duties, like ongoing monitoring of lab values, adjusting IV fluid drips according to the patients’ vital signs, and working with various teams, such as physical therapy, occupational therapy and respiratory therapy.
I frequently assist in transferring my patients to the operating room or for CT scans and MRIs, or even assisting in bedside procedures, like intubations, chest tubes and central line insertions. In addition to providing care to patients, we are providing education and support services as needed to their families.
The types of patients we treat in the ICU can range from respiratory care, oncology care, organ transplantation, surgical patients and more. As such, we collaborate with interdisciplinary teams on a daily basis, such as interventional radiology, surgery, oncology, pulmonology and others.
My day starts out about the same each morning, but then looks different as the day progresses and changes hour by hour; however, my entire 12-hour shift requires critical thinking at all times. At the end of a shift, a huddle takes place again for the oncoming shift. I then handoff to the night shift nurse, the same as how I started my day.
What is the difference between an ICU nurse and an Emergency Department nurse?
The best way to explain this difference is using a scenario. Let’s say a patient is having trouble breathing, complaining of chest pain and shortness of breath and calls 9-1-1 for emergency medical services (EMS). EMS transports the patient to the Emergency Department. There, the nurses are going to draw blood to send to the lab, make sure the patient’s blood pressure is stable, check oxygen levels and overall make sure to identify if any immediate interventions are needed. As soon as all of those diagnostics and interventions are completed, the physician in the Emergency Department will decide if a patient needs to remain in the hospital for additional testing and care.
If hospitalization is recommended, and depending on what type of medical interventions are needed, a patient may be transferred to the ICU. There, a group of specialized personnel will collaborate to provide the best and most updated care, and continue to diagnosis and treat the patient’s medical issues. We will continue to draw blood for labs and completes tests, stabilize the patient and provide them with intensive care over a period of time depending on the diagnosis.
What is the hardest part about being a nurse in the ICU?
We see many patients and their family members during the most vulnerable times in their lives. By far, the hardest part is witnessing a patient pass away due to their illness. We will perform all necessary and wanted life-saving measures, but at times, we have done all that we can. What makes this even more challenging is in those moments after witnessing a passing, I continue to provide support for other patients that are still in need and at that same high-level of care they deserve.
It’s in these moments I’m so grateful for my coworkers as we go through this together. When there are hard times at work, we are well-equipped to give a colleague a moment to recompose themselves and reflect. We are there for one another every day and lift each other up during those difficult, often emotional moments.
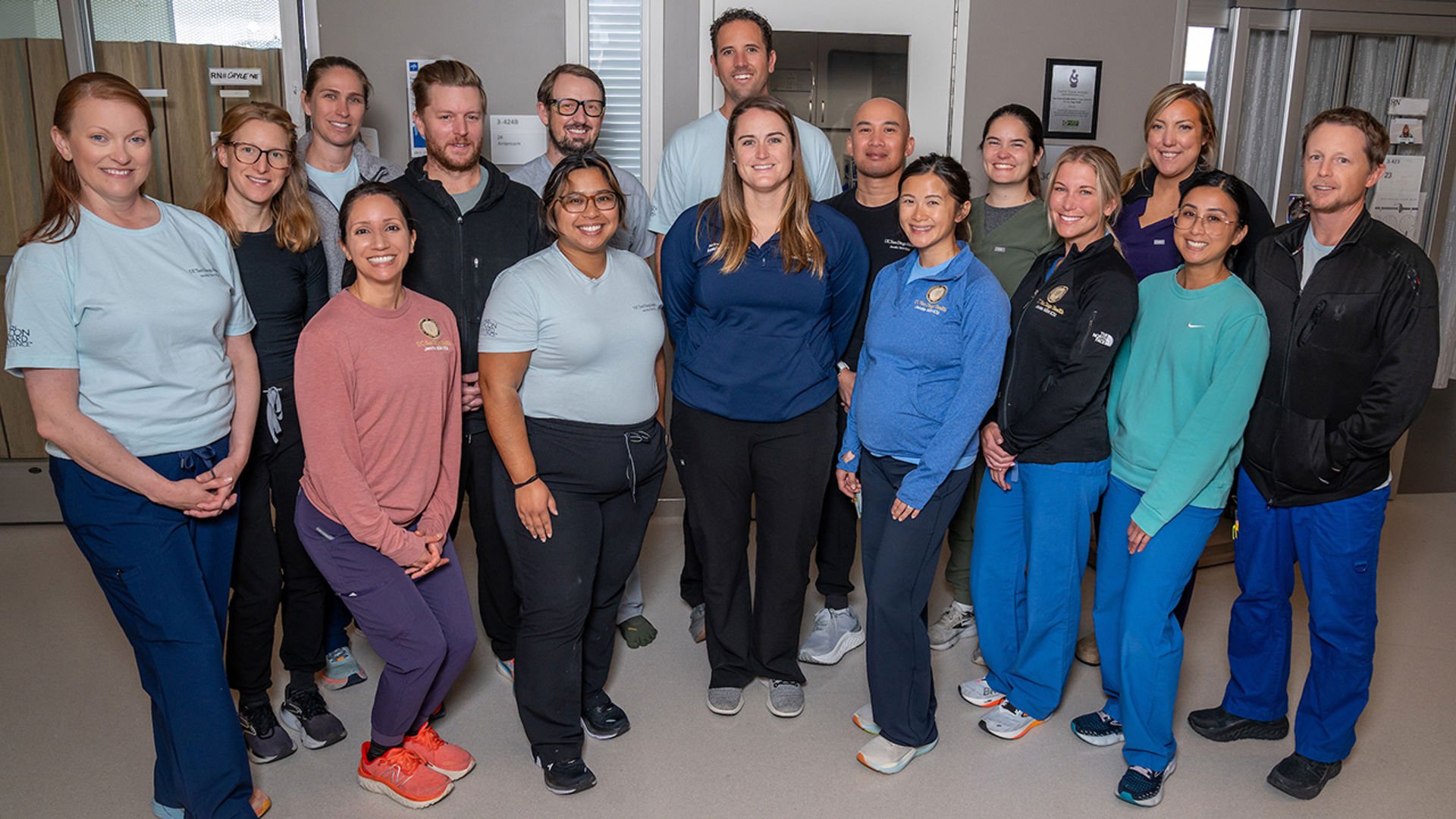
The award the ICU unit recently received from the AACN is a direct reflection of the interdisciplinary, collaborative environment developed at UC San Diego Health. Photo credit: Alex Matthews, UC San Diego Health
Why do you love being a nurse in the ICU?
I’ve been at UC San Diego Health for eight years now and have been working at the ICU at Jacobs Medical Center since it opened in 2016. I love what I do. The ICU provides me with a level of critical thinking in which I thrive on and offers these crucial moments where I feel I can make the biggest impact in the lives of our patients and their families.
Plus, the teamwork between our 3GH team is truly incredible; we are a family and we are always there to support one another. The award we recently received from the AACN is a direct reflection of the interdisciplinary, collaborative environment we’ve developed at UC San Diego Health.
Our nurses are involved with hospital-wide and unit-specific committees, along with a nursing governance board that works together as a team to make decisions for patients and staff, all with the shared vision and goal to treat patients like family and put their care first.
Receiving Support in the Intensive Care Unit
The need for critical care can be traumatic for a patient and their loved ones. We ensure a healing environment, as well as clear, compassionate and timely communication. Our goal is to involve and support each patient and their family in the caring process to enhance your recovery.


