Deep Vein Thrombosis & Pulmonary Embolism
Deep vein thrombosis (DVT) is a condition where blood clots form in the deep veins of the legs.
Deep vein thrombosis causes a pulmonary embolism when the clots break off, travel up to the lungs and get stuck in the arteries, creating a blockage.
Venous thromboembolism is a term that includes both pulmonary embolism and deep venous thrombosis. It can be provoked by a combination of hereditary and acquired risk factors.
Symptoms of DVT
Some people have no symptoms when clots form in their legs, while others have severe, debilitating symptoms. Deep venous thrombosis usually affects deep veins in the thigh, lower leg and pelvis, and less commonly, the arm.
People with deep venous thrombosis may have one or several of the following symptoms in the affected area:
- Tenderness
- Leg pain
- Redness and changes in skin color
- Skin that is warm to the touch
- Leg swelling
Symptoms of Pulmonary Embolism (PE)
Shortness of breath is often the first warning sign of pulmonary embolism. Since this can result from many different lung problems, it's important that you meet with a specialist who can provide an accurate diagnosis.How we check lung function
Some people with pulmonary embolism may also experience chest pain that is:
- Sharp and stabbing
- Worse as you breathe deeply
- On one side or underneath the breastbone
- Dull, aching or burning
Other symptoms that may indicate pulmonary embolism include:
- Fast heart rate
- Sudden cough
- Coughing up blood
- Clammy skin, excessive sweating
- Low blood pressure
- Bluish skin
- Fainting or dizziness
- Anxiety
If you have any of these symptoms, go to the ER or call 911
Often, a diagnosis is made in the emergency room (by a doctor and radiologist) when symptoms demand immediate medical care.
Lifesaving Pulmonary Embolism Care
A pulmonary embolism that does not resolve on its own can be life-threatening. For these cases, medication or surgery (rarely needed) is used to break up the clot.
There are two goals of pulmonary embolism treatment:
- Keep the existing blood clot from causing damage
- Prevent the formation of new clots
Anticoagulant Medicines
A pulmonary embolism is typically treated with anticoagulants, or "blood thinners." Despite its nickname, anticoagulants don't actually thin your blood — they stop your body's ability to clot. This helps keep existing clots from getting bigger.
While anticoagulants do not break up clots that have already formed, your body can usually dissolve clots on its own over time.
Anticoagulants come in the following forms:
- Pill (e.g., apixaban, rivaroxaban, dabigatran, warfarin)
- Injection (e.g., enoxaparin, dalteparin, fondaparinux)
- Intravenously (e.g., heparin)
Newer oral anticoagulants (e.g., apixaban, rivaroxaban, dabigatran) that do not require monitoring are available for some patients with a low risk of bleeding. Read About Our Anticoagulation Services
Other Treatments
Other forms of treatment may be necessary in cases when:
- The pulmonary embolism causes critical illness
- You are unable to take anticoagulant medicines
In these situations, the following therapies may be recommended:
Tissue plasminogen activator (tPA): A clot-dissolving medication.
Ultrasonic catheter: Administered by an interventional radiologist. Helps break up clots with ultrasonic waves. Often used jointly with tPA.
Surgical embolectomy: Blood clot is removed with surgery.
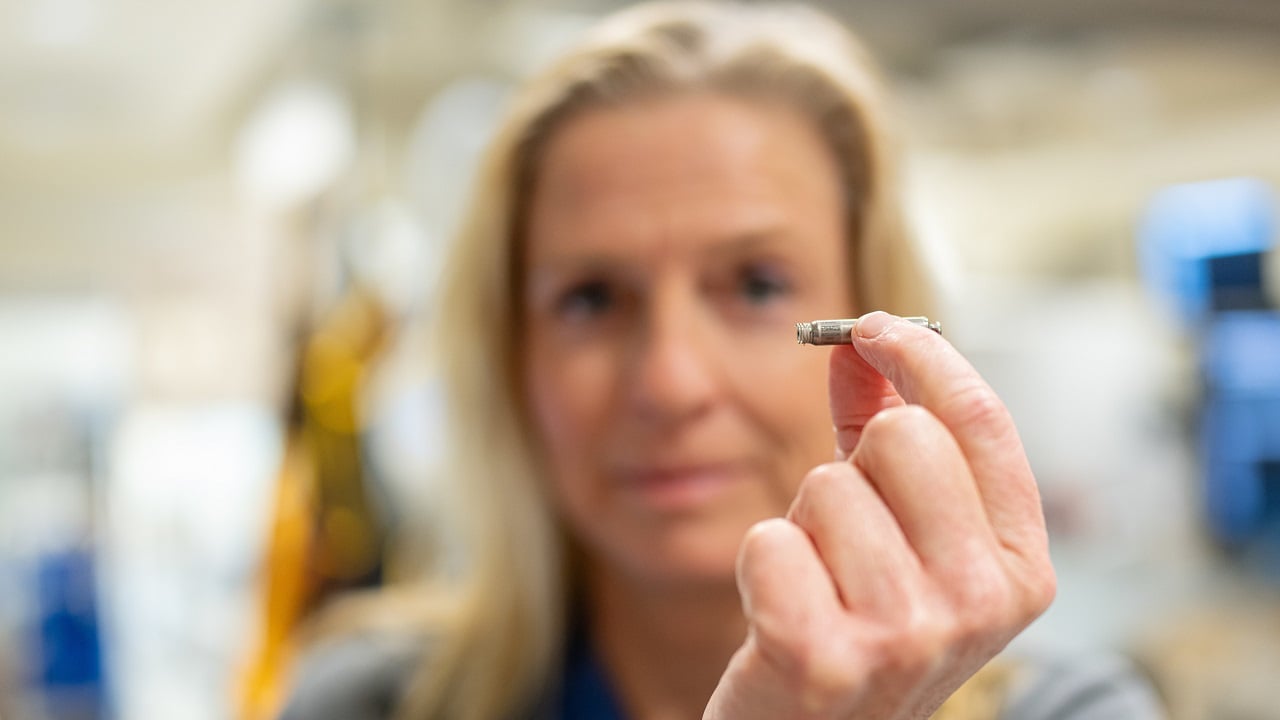
Vacuum catheter: A tiny vacuum is threaded through the veins and used to draw out blood clots.
Inferior vena cava (IVC) filter: A small, cone-shaped device designed to catch blood clots is implanted by an interventional radiologist in the inferior vena cava, the large vein that carries blood back to the heart, using a catheter. This minimally invasive procedure is done while the patient is awake.
An IVC filter can be permanently or temporarily implanted. While an IVC filter cannot prevent new blood clots from forming, it can help prevent deep venous thrombosis from moving into your lungs. Vena Cava Filter Implantation
Nearly one-third of people with acute pulmonary embolism will have some amount of scarring in the lung arteries that can cause chronic problems. In a small portion of these cases, scarred lung arteries eventually develop into chronic thromboembolic pulmonary hypertension (CTEPH). Learn About Our Groundbreaking Treatments for CTEPH
Long-Term Management After Pulmonary Embolism
Meeting with a specialist who can determine your risk for more blood clots and diagnose the cause of your shortness of breath may reduce your need for invasive surgeries later.
The pulmonary embolism experts at UC San Diego Health:
- Pinpoint the cause of your blood clot
- Ensure you have completely recovered from the blood clot
- Select the best therapy for you
- Assess your risk of recurrence
- Manage your anticoagulants around future operations
- Perform diagnostic testing (in the event you have shortness of breath)
The most important aspect of long-term care after a pulmonary embolism is reducing the risk for recurrent pulmonary embolism.
Blood Clot Risk
To fully assess your risk of blood clot recurrence, our team may:
- Develop a thorough history in order to determine the risk of future blood clots.
- Do blood tests to see if you have hypercoagulability (a tendency to form clots).
- Perform additional imaging tests.
After calculating your risk, we will work with you to determine a personalized preventive plan that includes recommendations for medication and length of treatment.
Shortness of Breath
After pulmonary embolism, some people continue to experience shortness of breath. If you're having symptoms of breathlessness, it's important that you follow up with a specialist who can properly evaluate your condition and rule out recurrent pulmonary embolism.
Other Prevention Tips for DVT
You can help prevent deep venous thrombosis by:
- Limiting the amount of time you spend in bed when ill or recovering from surgery.
- Taking medicines that help prevent blood clots (e.g., anticoagulants).
- Regularly participating in physical activity.
- Exercise/move leg muscles when forced to sit for long periods of time.
- Wearing compression stockings that promote blood flow in your legs.
Clinical Research
Our physician-scientists are active in clinical research, including clinical trials investigating:
- Prevention of blood clots following hospitalization
- The link between acute pulmonary embolism and CTEPH
We also participate in registry studies for pulmonary embolism. These studies allow us to gather data from multiple accredited medical centers to help provide a clearer understanding of the disease progression of pulmonary embolism and outcomes for different therapies.More about clinical trials at UC San Diego Health